Diabetic Foot & Foot Care, Treatments
What is Diabetes?
Diabetes is a medical condition that affects how the body uses glucose (sugar), which is the main source of energy for cells. Glucose comes from the food we eat and is transported through the bloodstream to cells throughout the body. Insulin, a hormone produced by the pancreas, helps to regulate the amount of glucose in the bloodstream by allowing cells to absorb and use glucose for energy.
In people with diabetes, the body either doesn’t produce enough insulin or can’t effectively use the insulin it does produce, leading to elevated levels of glucose in the bloodstream. This can cause a range of symptoms and health problems, including:
- Increased thirst and urination
- Hunger
- Fatigue
- Blurred vision
- Slow healing of cuts and wounds
- Numbness or tingling in the hands or feet
- Increased risk of infections and other health problems, such as heart disease, kidney disease, and nerve damage.
There are several types of diabetes, including type 1 diabetes, type 2 diabetes, and gestational diabetes. Treatment for diabetes typically involves lifestyle modifications, such as a healthy diet, regular exercise, and maintaining a healthy weight, as well as medications, such as insulin or oral medications, to help regulate blood sugar levels.

Symptoms of Diabetes
The symptoms of diabetes may vary depending on the type of diabetes, and some people with diabetes may not experience any symptoms at all. However, common symptoms of diabetes may include:
- Increased thirst and urination
- Fatigue or weakness
- Blurred vision
- Slow healing of cuts and wounds
- Numbness or tingling in the hands or feet
- Frequent infections, such as gum or skin infections
- Unintentional weight loss (in type 1 diabetes)
- Increased hunger, even after eating (in type 2 diabetes)
- Dry mouth and itchy skin
- Nausea and vomiting
It’s important to note that these symptoms may also be associated with other health conditions, so it’s important to seek medical attention if you experience persistent or severe symptoms. If left untreated, diabetes can lead to a range of health problems, including heart disease, kidney disease, nerve damage, and blindness.
Symptoms of Diabetes
Risk factors that Cause Diabetes
There are several risk factors that can increase the likelihood of developing diabetes, including:
- Family history: Having a close relative, such as a parent or sibling, with diabetes increases the risk of developing the condition.
- Obesity: Being overweight or obese can increase the risk of developing type 2 diabetes.
- Sedentary lifestyle: Lack of physical activity or a sedentary lifestyle can increase the risk of developing type 2 diabetes.
- Age: The risk of developing type 2 diabetes increases with age, particularly after the age of 45.
- Race or ethnicity: Certain racial and ethnic groups, including African Americans, Hispanic/Latino Americans, and Native Americans, have a higher risk of developing diabetes.
- Gestational diabetes: Women who develop gestational diabetes during pregnancy have a higher risk of developing type 2 diabetes later in life.
- Polycystic ovary syndrome (PCOS): Women with PCOS, a hormonal disorder that affects the ovaries, have a higher risk of developing type 2 diabetes.
- High blood pressure: Having high blood pressure, or taking medications to treat high blood pressure, can increase the risk of developing type 2 diabetes.
- High cholesterol: Having high levels of LDL (“bad”) cholesterol or low levels of HDL (“good”) cholesterol can increase the risk of developing type 2 diabetes.
- Smoking: Smoking cigarettes can increase the risk of developing type 2 diabetes and other health problems.
It’s important to note that having one or more of these risk factors does not necessarily mean that a person will develop diabetes, and there are also people who develop diabetes without any known risk factors. However, understanding these risk factors can help individuals make lifestyle modifications or seek appropriate medical care to help reduce their risk of developing diabetes.
Checklist for Managing the Symptoms of Diabetes
Check the footwear– Everyone should wear shoes that fit well and support their feet. The shoes should be low-heeled, supportive, and wide enough so that they can accommodate the foot. In addition to this, one needs to make sure that they don’t rub or pinch any area of the foot. Ideally, they must be lined with a soft and seamless interior. Worn-out shoes or those which do not fit properly often lead to foot complications.
Protect feet- One must protect their feet both inside and outside the home. Always wear slippers with a hard sole or sandal to protect the feet from any injury. Furthermore, it is also suggested to wear socks for added protection.
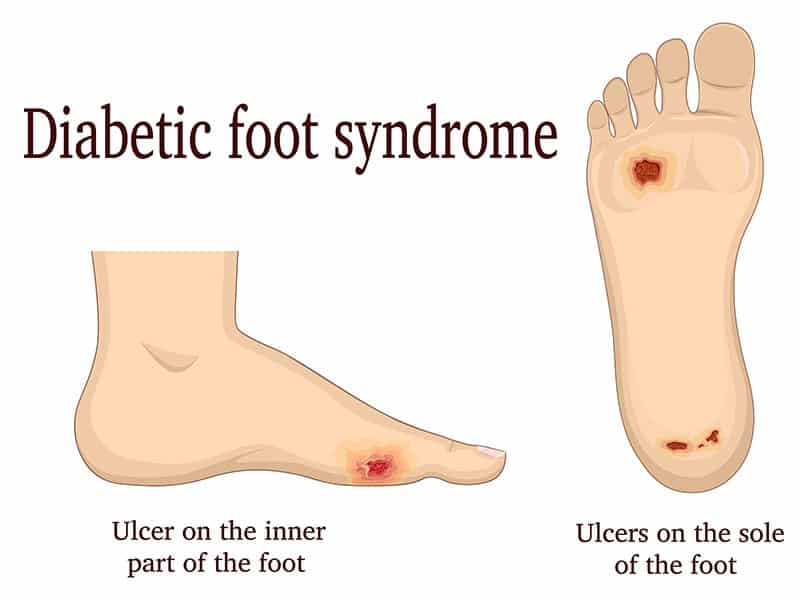
Examine the toes and feet daily- Check the skin regularly for any redness, blisters, cracks or dry patches. Inspect the toenails for cracks, sharp edges or any other changes
Maintain a healthy lifestyle– Healthy eating, management of blood glucose level, and weight control are three essential factors for successful diabetes management. Consult a dietician, family doctor or a diabetes care specialist for more information.
Diabetic foot care center in Delhi For custom foot orthotics
A custom orthotic is the most effective tool for preventing foot injury in people with diabetes. Unlike other conditions, where orthotics are used for correction or control, orthotics for diabetes require redistributing pressure along the soles of feet for reduction of areas where the patient experiences excessive pressure, friction, or shear.
At www.superfeetinsole.com, we offer custom orthotics that are manufactured specifically for you by using a 3D cast of your foot. Our foot experts design the orthotics with materials and additions in accordance with your needs. The orthotics are designed to offer you maximum convenience and comfort. As the best diabetic foot care we make sure our custom-made orthotics provide the most comfort and relief of symptoms. we also offer our services in allover India by using 3D technology.
Order your foot insoles now!


